9 hours ago
Monday, November 01, 2010
I Remember
[From Roger Ebert's Journal by way of Daring Fireball.]
OK, I don't post often lately. But I think remembering is important. Voting is, too. I encourage you to do both.
Tuesday, June 29, 2010
Really cool
I see that Practice Fusion is showing a "sneak preview" of their iPhone app on their Facebook page.
How cool would that be if I could access my patients' charts with just my iPhone? Especially when I'm on vacation like now.
Answer: Really cool.
How cool would that be if I could access my patients' charts with just my iPhone? Especially when I'm on vacation like now.
Answer: Really cool.
Location:Unseo-dong,Incheon,South Korea
On Vacation

I'm currently in Seoul, South Korea waiting for our connecting flight to Beijing. I'm taking a 2 week trip to China with my family. I thought this was an optimal time to go with my aging parents, who are from China, and my two teenage daughters, one of whom will be headed to college next fall. There won't be many chances for us to do this again.
I want to show that even though I have a solo micropratice, that I can still take vacations. All it takes is a friendly colleague willing to cover for me (thanks, Tom!), and Internet access. Free, if possible.
I'll post more details later on how I take care of business even when I'm out of the country. Assuming my hotel has free wifi access, that is.
Location:Unseo-dong,Incheon,South Korea
Tuesday, June 15, 2010
Really Retro
To match my retro solo family practice, I figure I should get myself one of these. Right after I get my iPad, that is.
And my iPad comes as soon as Practice Fusion can port their EMR over to the iPad. Even though it currently requires Adobe's Flash to run, Practice Fusion is hopefully coming to the Flashless iPad soon. According to their Facebook feed:
We'll be testing a wide variety of hardware and systems in the lab - including the iPad once our mobile strategy is closer to launch this year.
Thursday, April 22, 2010
Me and My Shadow, Part 6
My last two posts have been what medical students have been saying about my micropractice. Now, a short commentary about medical students and the future of family medicine. It has been well documented that fewer and fewer medical students are choosing to enter primary care specialities, such as family medicine. In order to combat this, there has been an effort in some circles to expose more medical students to family medicine, such as by requiring them to do a clinical clerkship in a family medicine office. I guess the logic is that if they see how great and fulfilling it is to be a family doctor, then more of them will want to go into it as a career.
As well-intentioned as this may seem, it has occurred to me that this may actually be counter-productive. There is no better way to turn off medical students from going into primary care than by having them see first-hand how frazzled, frustrated and overworked a primary care doctor's life really is. If you really want students to go into primary care, have them rotate through an office where there is enough time to talk with patients, where doctors are not overworked, and where both doctors and patients are happy. But you won't find many places like that in the current environment. That is why you won't see any signicant increase in primary care doctors until the lives of primary care doctors are improved. And that ultimately means: more money for primary care.
As well-intentioned as this may seem, it has occurred to me that this may actually be counter-productive. There is no better way to turn off medical students from going into primary care than by having them see first-hand how frazzled, frustrated and overworked a primary care doctor's life really is. If you really want students to go into primary care, have them rotate through an office where there is enough time to talk with patients, where doctors are not overworked, and where both doctors and patients are happy. But you won't find many places like that in the current environment. That is why you won't see any signicant increase in primary care doctors until the lives of primary care doctors are improved. And that ultimately means: more money for primary care.
Returning to the present and vowing not to repeat the delays of my last two posts, I will now share what my latest medical student wrote just last week. Analisa just completed her 5 week family medicine clinical clerkship with me and was kind enough to share her thoughts about my practice model. Kudos to her for writing this during her trauma surgery rotation!
The first time I met Dr. S was not as a medical student. I first found his practice as a patient. I was new to the area and needed a vaccination booster. His practice was close by and gave vaccinations. So, I researched this new office discovery. I found his practice model intriguing and the level of care incredibly personal. Three years later, I was back in Dr. S’s office to learn more.Thank you, Analisa, for your enthusiasm, hard work and desire to learn. (Also your willingness to do administrative chores when things were slow.) You were able to handle anything I threw to you, so I am confident you will excel in whatever you end up choosing to pursue. Best wishes to you!
Initially, I knew Dr. S modeled a practice without the usual constraints of time and bureaucracy. Following the ideal medical practice model tenets of efficiency, quality, and care access, Dr. S offered a hope for something beyond the fast paced, quick in and out practice with which I had more experience. In Dr. S’s office, I was able to talk to patients. I was able to carry out a full conversation discussing the spectrum of life experiences that were either aiding or impeding wellness. We did not see many patients a day, and thus, when complications in patient care arose, we were able to be proactive and address concerns before they snowballed into something bigger.
Seeing patients with Dr. S was somewhat like the 1940s TV depiction of the town doctor whose neighbors came by with a cough, an ankle sprain, or anything really. Experiencing the paradigm of neighborhood doctor as confidant, consultant, and medical expert was rewarding.
Further, this personal care was enhanced with the aid of technology. I appreciated the efficiency of Dr. S’s near paperless office were patients could schedule their own appointments online and encrypted patient information was physician accessible, fully incorporated and well organized.
Some patients just needed a quick check up. Some patients needed more. Dr. S was there for his patients, whatever their concerns. I was impressed with the same day appointments, the evening appointments, the occasional weekend appointment, and the consistent email contact. I was impressed by the patient driven care.
As I move forward in my career, the principles of the ideal medical practice will stay with me. Dr. S’s insight into the importance of creating the medical practice for the kind of medicine you believe should be practiced is no doubt a lesson worth retaining.
Analisa Armstrong, MS3
Wednesday, April 21, 2010
Me and My Shadow, Part 5
As I mentioned in yesterday's post, I am ashamed to say that I have been sitting on a couple of essays from medical students who rotated with me since 2007-2008. I kept meaning to post them but time just sort of slips away and before you know it, it's the next decade. So with apologies to Erin for the late posting, here are her thoughts on her 5 week rotation with me from 2008:
One positive consequence of posting this 2 years late is that I can look up what has happened to Erin since then. Upon graduation from the USC Keck School of Medicine last year, she was honored with the American College of Physicians Regional Student Award. She is now finishing her 1st year of internal medicine residency at UCLA. Congratuations, Erin! Only 8 more years to go to find out if she has her own micropractice.
Tomorrow: Me and My Shadow, Part 6: Analisa's Clerkship
I did not know what to expect when I discovered that Dr. S’s family medicine practice was a “micro-practice”. I had never even heard of a micro-practice and I assumed it was just another word for “concierge service”. My doctor in the Bay Area recently made the change to concierge service. She does not take insurance and charges $400/month; however she recommends having insurance to pay for labs, hospital stays, etc. ($5000 a year + insurance payments!? Is she crazy?). In my opinion these concierge services cater to the rich – and cater to themselves. Therefore, I had an unfounded preconceived notion about Dr. S’s practice before I even got there. I wasn’t upset about working for this kind of practice, I was excited to see something different, and most importantly, I did not have to drive through traffic to get to his office.
I was certainly wrong about micro-practices. They are not concierge services. A micro-practice is almost a nice blend between concierge and standard practice. You get the outstanding service that a concierge practice offers and the practicality/price of a standard practice (ie: he takes insurance). Moreover, Dr. S does everything himself.. Answering the phone, billing, scheduling, taking vital signs, etc, etc. It is this aspect of a micro-practice that I do not like.
Honestly, I was annoyed having to take the blood pressure and the heart rate of most patients. I have never had to do this before. I was also embarrassed at my annoyance. When did I become so entitled? Isn’t it my job as a medical student to do these basic skills and be competent at them? Before I worked with Dr. S, I had maybe taken vital signs myself a total of four times. I had gotten spoiled, I had gotten lazy . . . I really needed this kick to bring me back to earth. I am after all, a medical student.
Dr. S certainly has patience and it makes me wonder if I would have the patience to do a micro-practice. I really like the idea of a micro-practice, but I don’t know if I could make the sacrifices it takes to start one. It really takes faith. His calendar is often empty at the start of the week. I am a very type A personality, so it drove me crazy not ever knowing when we were going to have patients. I also would get nervous that no one would call. How does Dr. S stay so calm? Inevitably, his appointments would fill – but it was the sense of unknowing that was really difficult for me to handle.
Despite these problems, overall my training was very rewarding. The most satisfying part of this practice was spending time with the patients. I felt I had a lot of autonomy and I really felt like I was part of the health care team. By the end of my time there I was confident in diagnosing and managing basic family care problems. I really loved that I could spend 30 minutes with a patient. I loved not feeling rushed and not having to constantly check my watch and think about how late I was with my appointments. Educating a patient is a very rewarding task. I have never had the opportunity before to really educate the patient about their disease and help them understand what was wrong. Doing this really involved the patient in his or her own health care – which I think is a vital step to success. I actually felt good about myself after many encounters – which is funny because it was almost as if the patient was helping me just as I was helping them.
In terms of medical training, I think his practice is a fantastic learning environment. There are some down sides that medical students have to accept: the quantity of patients seen is low compared to other practices (however, the quality is equal if not better). If you are a student that learns by seeing the same thing over and over again, then perhaps this is not the best practice for you to learn at. However, if you are a student that learns by discussing the case afterwards in extraordinary detail and following up on it with textbook and literature searches – then his practice is ideal. We always had time to discuss each patient. I really felt like I understood WHY I was prescribing a particular treatment because we would compare the possible options and use evidence based medicine to re-affirm our decision. I really enjoyed this because I felt like I was not blindly giving out treatments because of recognition pattern, but that I was rationally choosing them. I was never afraid to ask a question and the best part is that he always had an answer.
After my five weeks with Dr. S I am certain about one thing: when I am no longer stuck using student health insurance, I will only go to a micro-practice family medicine doctor. This type of practice is the best option for a patient. The service and quality of care cannot be beat. The uncertainty lies in whether I would ever run a micro-practice. It is definitely a possibility and ideally I would want to. However, idealism and practicality are two different things. Call me in 10 years and I will let you know.A belated thanks for your thoughts and insights, Erin.
Erin Atkinson, MS3
One positive consequence of posting this 2 years late is that I can look up what has happened to Erin since then. Upon graduation from the USC Keck School of Medicine last year, she was honored with the American College of Physicians Regional Student Award. She is now finishing her 1st year of internal medicine residency at UCLA. Congratuations, Erin! Only 8 more years to go to find out if she has her own micropractice.
Tomorrow: Me and My Shadow, Part 6: Analisa's Clerkship
Tuesday, April 20, 2010
Me and My Shadow, Part 4
Periodically I have a medical student do a clinical rotation with me and at the end, I ask them to write an essay about their experience working with me in my micropractice. I am ashamed to say that I have been sitting on a couple of essays since 2007-2008. I kept meaning to post them but time just sort of slips away and before you know it, it's the next decade. So with apologies to Andrew for the late posting, here are his thoughts on his 5 week clerkship with me from October 2007 (all the more impressive because he wrote this during his surgery rotation!):
A belated thank you, Andrew, for your thoughts and honest opinions.
One positive consequence of posting this 2 years late is that I can look up what has happened to Andrew since then. He was selected as one of the participants in USC Keck School of Medicine Dean's "Year for Research" Program for Medical Students for 2008-2009, doing research in orthopedic surgery in Pittsburgh.
I suspect he is now finishing his 4th year, preparing to graduate from medical school, and getting ready to pursue his dreams. Good luck, Andrew, and I hope you find that ideal balance between career and personal life. This is the wish I have for all physicians. And, of course, especially for solo docs.
Tomorrow: Me and My Shadow, Part 5: Erin's Clerkship
I am just starting the fifth week of my surgery rotation at the Keck School of Medicine at USC. These past four weeks have been a very exciting time for me, as surgery has been my career of choice since I applied to medical school. At the same time, when I left Dr. S’s office four weeks ago, I was sad to leave what was an extremely educational experience and what became a very comfortable environment for me. From a medical student standpoint, I must be honest about my initial expectations of family medicine. Not knowing much about the specialty, I unfairly assumed that the patient cases would get repetitive and uninteresting. I figured that the rotation would be simply another roadblock between me and my career as a surgeon.
Now, after completing the rotation, I am thankful of two things. First, that my assumptions were, for the most part, wrong. (Actually, I will say that some of the patient cases got repetitive such as common colds, strep throat, annual physicals, flu shots/immunizations, etc. Such cases may not be as interesting or complicated as the heart valve replacements I have seen most recently, but I suppose even those cases may at some point become repetitive as well.) Second, that my experience with Dr. S changed a roadblock into a gateway. I was introduced to the “art of medicine,” where being a good doctor was not about the ability to diagnose a patient with diabetes but more about the ability to perform a comprehensive examination of each patient while taking the time to connect with patients on a more personal level.
From a medical student’s perspective, I found Dr. S’s practice to be unique and in a way… idealistic. In our first and second years of medical school, we are taught to perform the idealistic patient interview and physical exam that, when done thoroughly, take anywhere from 30 minutes to 1 hour to complete. We are also trained in the skills of bedside manner. When our actual clinical years of training begin during third year, we throw away two years of instruction, and instead fumble through 10-15 minute interviews/physicals. Sad as it may be, that is exactly what happens to most medical students. Fortunately, I was given the opportunity during my family medicine rotation to experience the ideal patient encounter. I can see how this model of family practice provides doctors with greater satisfaction and enjoyment over the style that forces physicians to see a larger volume of patients.
From a personal perspective, learning about micro practices has opened up new career possibilities. More and more I am discovering how much I enjoy life outside of my career. While I am almost certain surgery will continue to interest me, I am equally certain that my family and social life outside of medicine will become (if it is not already) more important to me. Weeks into my surgery rotation, I am realizing that surgery will most likely require my attention full-time or for even longer hours, while family medicine, especially micro and concierge type practices afford much more flexibility in time.
Though I am even more conflicted now about choosing a medical specialty, I am glad to have had such a unique opportunity with Dr. S. So I will close this entry by saying thank you, and I hope in the future to have the opportunity to write of my own experiences with private practice if that is where my career takes me.
Andrew Wong, MS3
A belated thank you, Andrew, for your thoughts and honest opinions.
One positive consequence of posting this 2 years late is that I can look up what has happened to Andrew since then. He was selected as one of the participants in USC Keck School of Medicine Dean's "Year for Research" Program for Medical Students for 2008-2009, doing research in orthopedic surgery in Pittsburgh.
I suspect he is now finishing his 4th year, preparing to graduate from medical school, and getting ready to pursue his dreams. Good luck, Andrew, and I hope you find that ideal balance between career and personal life. This is the wish I have for all physicians. And, of course, especially for solo docs.
Tomorrow: Me and My Shadow, Part 5: Erin's Clerkship
Friday, March 26, 2010
Recap: Pay What You Can Day
So despite my attempts to publicize the offer to provide "Pay What You Can" medical care for a day, I ended up seeing 4 patients that day (with one cancellation). The other doctor doing this with me, Dr. Tsai, also saw 4 patients, and we agreed that though the numbers seemed low, we were thankful not to have been overwhelmed by too many patients.
I think the patients I saw were grateful to receive medical care, and I was happy to help them and not worry about money. Still, I was pleasantly surprised to find that most patients paid something for their visits, even though they didn't have to pay anything at all.
I may see some of these patients again, depending on what we can work out. I talked about potentially bartering services with one patient in lieu of cash.
Dr. Tsai and I weren't the only doctors doing "Pay What You Can Medical Day". Dr. Jean Antonucci in Maine also invited patients to come in for medical visits and pay whatever they could for a day. Here is the local TV coverage for her day:
And for those who can't watch the video, here is the link to the print version.
Some may argue whether it is even worth it to give away medical care for just one day and that patients don't get free labs, medications or follow up care.
For labs and mammograms, I directed patients to the cheapest facility that offered cash discounts. For medications, I prescribed $4 generics whenever I could. I will notify patients of their test results for free, but future visits would be negotiable.
Even humanitarian efforts such as sending medical personnel to Haiti after their devastating earthquake (where Dr. Tsai volunteered) or the Remote Area Medical event which helped 6,400 people in August 2009 and which is coming back to Los Angeles in April 2010 don't provide any long-term solution to medical care, but no one is arguing that these efforts are a waste of time.
We each do what we can to help others, whether it be to provide free medical care for a day, or committing your entire life to caring for the poor and sick, or just giving a word of encouragement.
Next year, I will get the word out sooner so that this event will be able to reach more people.
I think the patients I saw were grateful to receive medical care, and I was happy to help them and not worry about money. Still, I was pleasantly surprised to find that most patients paid something for their visits, even though they didn't have to pay anything at all.
I may see some of these patients again, depending on what we can work out. I talked about potentially bartering services with one patient in lieu of cash.
Dr. Tsai and I weren't the only doctors doing "Pay What You Can Medical Day". Dr. Jean Antonucci in Maine also invited patients to come in for medical visits and pay whatever they could for a day. Here is the local TV coverage for her day:
And for those who can't watch the video, here is the link to the print version.
Some may argue whether it is even worth it to give away medical care for just one day and that patients don't get free labs, medications or follow up care.
For labs and mammograms, I directed patients to the cheapest facility that offered cash discounts. For medications, I prescribed $4 generics whenever I could. I will notify patients of their test results for free, but future visits would be negotiable.
Even humanitarian efforts such as sending medical personnel to Haiti after their devastating earthquake (where Dr. Tsai volunteered) or the Remote Area Medical event which helped 6,400 people in August 2009 and which is coming back to Los Angeles in April 2010 don't provide any long-term solution to medical care, but no one is arguing that these efforts are a waste of time.
We each do what we can to help others, whether it be to provide free medical care for a day, or committing your entire life to caring for the poor and sick, or just giving a word of encouragement.
Next year, I will get the word out sooner so that this event will be able to reach more people.
Tuesday, March 23, 2010
Monday, March 22, 2010
The Trouble With Giving Away Free Health Care
It all started with a question: "How much do patients value primary care?"
I was having an online discussion with other primary care physicians and this question came up. Someone suggested that one way to find out was to offer medical visits and have patients pay whatever they thought the visit was worth. Okay, I said, I'll give it a try. But when?
For the past few years, I kept intending to do something as part of Cover the Uninsured Week, but never could figure out what I could do. This year, I thought, I could make this experiment part of that. But when I checked the Cover the Uninsured website, there was no date set for their annual Cover the Uninsured Week. Maybe they weren't having one this year?
So I dragged my feet. Then on March 10th I checked the Cover the Uninsured website one more time and whoops! Cover the Uninsured Week was suddenly the next week! When did they decide that?
I had to make some quick decisions. I decided to have a one day event on March 23rd because that was during Spring Break; I wouldn't need to pick up my kids from school and I could stay all day at the office seeing patients.
I wrote up a press release to turn in to the local weekly newspaper. Their deadline was Friday and came out on Wednesday. That would allow a little more than a week for people to find out about it. I contacted another local family doctor who had just gone to Haiti to help in their relief effort to see if he would be interested in taking part. He was, so I added his name to the press release. I also sent the press release to the local chamber of commerce for distribution to local businesses, many of whom I figured would have uninsured employees, and a press release to the larger local paper.
Unfortunately, there was no link to the article on the main page of the newspaper, so the only way anyone could find it was to do a Google search. I e-mailed the press release to 3 more local TV stations but it was the weekend and I got no response. It was looking bleak. On the positive side, the healthcare reform bill was being passed by the House. On the negative side, I had only 3 patients scheduled for "Pay What You Can Day".
This morning I talked with the reporter again and he said that there was an article published in today's printed newspaper, and he would make sure that the article was posted with a link to the main page this time. And so he did:
Maybe everyone will call tomorrow morning. Or maybe a bunch of people will just walk in tomorrow. Or maybe, just maybe, nobody needs free healthcare right now?
I was having an online discussion with other primary care physicians and this question came up. Someone suggested that one way to find out was to offer medical visits and have patients pay whatever they thought the visit was worth. Okay, I said, I'll give it a try. But when?
For the past few years, I kept intending to do something as part of Cover the Uninsured Week, but never could figure out what I could do. This year, I thought, I could make this experiment part of that. But when I checked the Cover the Uninsured website, there was no date set for their annual Cover the Uninsured Week. Maybe they weren't having one this year?
So I dragged my feet. Then on March 10th I checked the Cover the Uninsured website one more time and whoops! Cover the Uninsured Week was suddenly the next week! When did they decide that?
I had to make some quick decisions. I decided to have a one day event on March 23rd because that was during Spring Break; I wouldn't need to pick up my kids from school and I could stay all day at the office seeing patients.
I wrote up a press release to turn in to the local weekly newspaper. Their deadline was Friday and came out on Wednesday. That would allow a little more than a week for people to find out about it. I contacted another local family doctor who had just gone to Haiti to help in their relief effort to see if he would be interested in taking part. He was, so I added his name to the press release. I also sent the press release to the local chamber of commerce for distribution to local businesses, many of whom I figured would have uninsured employees, and a press release to the larger local paper.
I decided at the time to limit it to only South Pasadena residents and employees of South Pasadena businesses because I didn't think we could handle it if there was a huge response.
Finally the article was published on Wednesday March 17th and . . . we waited. No one called. Friday morning, the chamber of commerce sent out an e-mail announcing the offer. One person called and scheduled an appointment.
OK, I thought, maybe I miscalculated. Either there aren't a lot of uninsured people in South Pasadena, or there wasn't a pressing need for medical care at this time. I mean, a one day offer of free medical care isn't going to cut it for chronic diseases such as diabetes or hypertension. Or the message wasn't reaching the right people. Our small town paper has a circulation, I'm told, of about 4000.
So I sent a modified press release to the local public radio station and a local TV station. This time, the offer was for anyone without insurance. Since I had no response from my press release, I called the local newspaper and spoke to a reporter who immediately sounded interested when I told him of our idea. But it was already late Friday morning and there wasn't enough time to come do an in-depth interview before the weekend. So he wrote up something quick and posted it to the website.
OK, I thought, maybe I miscalculated. Either there aren't a lot of uninsured people in South Pasadena, or there wasn't a pressing need for medical care at this time. I mean, a one day offer of free medical care isn't going to cut it for chronic diseases such as diabetes or hypertension. Or the message wasn't reaching the right people. Our small town paper has a circulation, I'm told, of about 4000.
So I sent a modified press release to the local public radio station and a local TV station. This time, the offer was for anyone without insurance. Since I had no response from my press release, I called the local newspaper and spoke to a reporter who immediately sounded interested when I told him of our idea. But it was already late Friday morning and there wasn't enough time to come do an in-depth interview before the weekend. So he wrote up something quick and posted it to the website.
This morning I talked with the reporter again and he said that there was an article published in today's printed newspaper, and he would make sure that the article was posted with a link to the main page this time. And so he did:
"South Pasadena doctors to give free medical care for a day"I've had one call so far from this article. It is 5:19PM. Hmmm. Still not looking so good.
Maybe everyone will call tomorrow morning. Or maybe a bunch of people will just walk in tomorrow. Or maybe, just maybe, nobody needs free healthcare right now?
Sunday, March 21, 2010
iPods and Healthcare Reform
In the late 1990s, an engineer named Tony Fadell came up with the idea of a hard drive-based MP3 player coupled with a Napster-like music store to complement it. He shopped the idea around to several companies but was turned down at all of them except for one. That company was Apple.
After modifying, improving, changing Fadell's original concept, Apple released a new device in 2001 they called an iPod.
The initial reaction on Slashdot, a prominent tech site gave this one sentence review:
And yet somehow the iPod went on to take over the music player industry. It now has about a 75% share of the market and has sold over 225 million units and counting.
It helped re-establish Apple as a top electronics brand, and paved the way for its subsequent successes with the iPhone and now the upcoming iPad.
The original iPod wasn't perfect. It was a start of something new, and it has improved gradually but continuously since then. But if Apple had listened to the naysayers and pundits at the time, none of this would have happened.
So I believe it will be with the current healthcare reform bill. It is not perfect, but there never could be such a thing as a perfect healthcare reform bill anyways. Those who criticize it and want it to fail because it doesn't have everything they want are short-sighted and unrealistic.
These are the same kind of people who couldn't see the potential in a little electronic music player, only the flaws.
If healthcare reform fails to pass now, it will be a loooonnnng time before any legislator attempts to try this again. And frankly, we can't afford to wait as the current system continues to crumble and cost everybody more and more money for worse and worse care.
As of now, I don't know if it will get the required votes or not, but I hope it passes. And if it does, I think it can be shaped and molded and upgraded over time to become a even better healthcare system.
After modifying, improving, changing Fadell's original concept, Apple released a new device in 2001 they called an iPod.
The initial reaction on Slashdot, a prominent tech site gave this one sentence review:
"No wireless. Less space than a nomad. Lame."At $399, it was also $150 more than a comparable $249 Nomad Jukebox. It wasn't compatible with Windows PC computers, just Macs which had a small market share at the time. You couldn't replace the battery. It had no FM radio. Many critics predicted it would flop.
And yet somehow the iPod went on to take over the music player industry. It now has about a 75% share of the market and has sold over 225 million units and counting.
It helped re-establish Apple as a top electronics brand, and paved the way for its subsequent successes with the iPhone and now the upcoming iPad.
The original iPod wasn't perfect. It was a start of something new, and it has improved gradually but continuously since then. But if Apple had listened to the naysayers and pundits at the time, none of this would have happened.
So I believe it will be with the current healthcare reform bill. It is not perfect, but there never could be such a thing as a perfect healthcare reform bill anyways. Those who criticize it and want it to fail because it doesn't have everything they want are short-sighted and unrealistic.
These are the same kind of people who couldn't see the potential in a little electronic music player, only the flaws.
If healthcare reform fails to pass now, it will be a loooonnnng time before any legislator attempts to try this again. And frankly, we can't afford to wait as the current system continues to crumble and cost everybody more and more money for worse and worse care.
As of now, I don't know if it will get the required votes or not, but I hope it passes. And if it does, I think it can be shaped and molded and upgraded over time to become a even better healthcare system.
Wednesday, March 10, 2010
The Family Practitioner
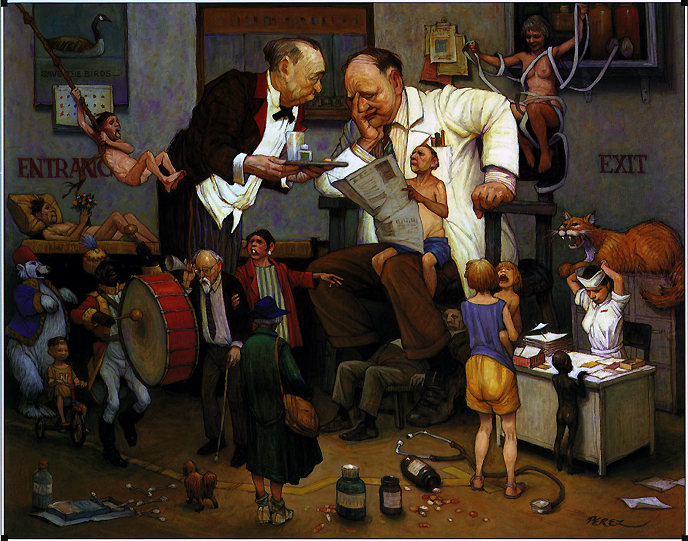
Found this illustration via The Examining Room of Dr. Charles. I'd say it captures the feel of most family doctors' offices just right except that the tape the woman sitting behind the doctor is tangled up in should be red instead of white.
For other depictions of various medical specialties, go to this exhibition on the art of Jose Perez.
Tuesday, March 09, 2010
A Top 50 Blog!
My blog is number 35 on this list which came out a while ago and is in no particular order. Amazing, considering how infrequently I post. But I am more about quality than quantity. That is, after all, why I left seeing 24+ patients a day and now see about 4-6 patients/day in my little micropractice.
Speaking of Top 50 blogs, I notice over on the excellent DB's Medical Rants site that he is posting his monthly workout tally on his blog, I guess to hold himself accountable for his exercise regimen. Likewise, over the past few years, I have come to the realization that I need to be pushed to exercise.
Like many of you, I had my gym membership that got used for the first few months, only to languish and fall to the wayside as my schedule got busy and motivation waned.
Then a few years ago, my wife showed me this newspaper article about a trainer that can help you dunk. I thought, why not give it a try? So I called the trainer up and he has been training me ever since. I haven't dunked a basketball yet (at least not on a 10 foot rim), but I have touched the rim, something I haven't done since college. In case you're wondering, I'm only 5'9".
But I am convinced that if I keep at it, I will eventually achieve my goal and dunk. Just like I was able to establish my solo micropractice. But I still need some coaching to help get me where I want to be.
That is what we can all use sometimes, whether is is losing weight, eating better, managing time, etc. A little coaching. And a willingness to work at it.
Speaking of Top 50 blogs, I notice over on the excellent DB's Medical Rants site that he is posting his monthly workout tally on his blog, I guess to hold himself accountable for his exercise regimen. Likewise, over the past few years, I have come to the realization that I need to be pushed to exercise.
Like many of you, I had my gym membership that got used for the first few months, only to languish and fall to the wayside as my schedule got busy and motivation waned.
Then a few years ago, my wife showed me this newspaper article about a trainer that can help you dunk. I thought, why not give it a try? So I called the trainer up and he has been training me ever since. I haven't dunked a basketball yet (at least not on a 10 foot rim), but I have touched the rim, something I haven't done since college. In case you're wondering, I'm only 5'9".
But I am convinced that if I keep at it, I will eventually achieve my goal and dunk. Just like I was able to establish my solo micropractice. But I still need some coaching to help get me where I want to be.
That is what we can all use sometimes, whether is is losing weight, eating better, managing time, etc. A little coaching. And a willingness to work at it.
Monday, March 08, 2010
The 7 Doctors and the Patient
Once upon a time, there were six doctors in a hospital. One day the admission clerk told them, "Hey, there is a patient in the hospital today."
They had no idea why the patient was in the hospital. They decided, "Even though we have no old chart, let us go and examine the patient anyway." All of them went to where the patient was. Every one of them touched the patient.
"Hey, this is atopic dermatitis," said the first doctor who touched his skin, for he was a dermatologist.
They had no idea why the patient was in the hospital. They decided, "Even though we have no old chart, let us go and examine the patient anyway." All of them went to where the patient was. Every one of them touched the patient.
"Hey, this is atopic dermatitis," said the first doctor who touched his skin, for he was a dermatologist.
"Oh, no! it is acute lumbago," said the second doctor who touched the back, for he was an orthopedic surgeon.
"Oh, no! it is paroxysmal tachycardia," said the third doctor who touched the chest of the patient, for he was a cardiologist.
"It is temporomandibular joint syndrome" said the fourth doctor who touched the jaw of the patient, for he was an otolaryngologist.
"It is spastic colitis," said the fifth doctor who touched the belly of the patient, for he was a gastroenterologist.
"No, it's lacrimal duct obstruction," said the sixth doctor who touched a tear from the eye of the patient, for he was a ophthalmologist.
They began to argue about the patient and every one of them insisted that he was right. It looked like they were getting agitated.
A seventh doctor was passing by and she saw this. She stopped and asked them, "What is the matter?" They said, "We cannot agree on the patient's diagnosis." Each one of them told what he thought the patient had.
The seventh doctor took a good look at the patient and said, "I know this man. This is Joe, and he is having an acute stress reaction because he just lost his job and his wife is being treated for breast cancer." And she shook his hand, offered some reassurance and made Joe feel better, for she was his family doctor.
Based on a well known story about an elephant.
"Oh, no! it is paroxysmal tachycardia," said the third doctor who touched the chest of the patient, for he was a cardiologist.
"It is temporomandibular joint syndrome" said the fourth doctor who touched the jaw of the patient, for he was an otolaryngologist.
"It is spastic colitis," said the fifth doctor who touched the belly of the patient, for he was a gastroenterologist.
"No, it's lacrimal duct obstruction," said the sixth doctor who touched a tear from the eye of the patient, for he was a ophthalmologist.
They began to argue about the patient and every one of them insisted that he was right. It looked like they were getting agitated.
A seventh doctor was passing by and she saw this. She stopped and asked them, "What is the matter?" They said, "We cannot agree on the patient's diagnosis." Each one of them told what he thought the patient had.
The seventh doctor took a good look at the patient and said, "I know this man. This is Joe, and he is having an acute stress reaction because he just lost his job and his wife is being treated for breast cancer." And she shook his hand, offered some reassurance and made Joe feel better, for she was his family doctor.
Based on a well known story about an elephant.
Sunday, March 07, 2010
3 hours vs 36 minutes
That's the difference between how much time my patients get with me per year vs a typical primary care practice, using the same kind of calculation from this article posted at kevinmd.com found by way of the Ideal Medical Practices blog.
Assuming 2 weeks of vacation a year and a patient panel of 500:
50 weeks a year x 30 hours per week divided by 500 patients = 3 hours.
Compare this to the 36 minutes per year patients get in a typical primary care doctor's office with a patient panel of 2500.
"I can see you today."
"I can see you on time."
"We can take all the time you want and need."
This is the mantra of the Ideal Medical Practice model.
Assuming 2 weeks of vacation a year and a patient panel of 500:
50 weeks a year x 30 hours per week divided by 500 patients = 3 hours.
Compare this to the 36 minutes per year patients get in a typical primary care doctor's office with a patient panel of 2500.
"I can see you today."
"I can see you on time."
"We can take all the time you want and need."
This is the mantra of the Ideal Medical Practice model.
Saturday, March 06, 2010
A Different Hat
I am currently in Sacramento wearing my California Academy of Family Physicians (CAFP) delegate hat at the Annual Congress of Delegates. Lots of civic-minded, concerned and caring family doctors doing a relatively thankless job. None of us get paid for this. Most family doctors in the state don't even know what we are doing at this meeting or that there is a meeting. But we are just trying to make a difference.
Dr. Lori Heim, president of the American Academy of Family Physicians, was the guest speaker and she gave a quick update of how she sees the current healthcare reform going in Washington, DC. She gives the current bill a 50-60 percent chance of making it into law.
She noted how much has changed since 1 year ago when everyone talked about the importance of healthcare reform and how cooperative and bipartisan the initial talk had been. Fast forward to now and, even after 20+ years of health policy debate and study, it has reverted back to being partisan in the ugliest way.
She outlined AAFP's priorities for health care reform:
Dr. Lori Heim, president of the American Academy of Family Physicians, was the guest speaker and she gave a quick update of how she sees the current healthcare reform going in Washington, DC. She gives the current bill a 50-60 percent chance of making it into law.
She noted how much has changed since 1 year ago when everyone talked about the importance of healthcare reform and how cooperative and bipartisan the initial talk had been. Fast forward to now and, even after 20+ years of health policy debate and study, it has reverted back to being partisan in the ugliest way.
She outlined AAFP's priorities for health care reform:
- Expand coverage with minimum benefits package
- Increase access/increase primary care workforce
- Insurance market reform
- Tort reform
Massachusetts demonstrated what happens when you increase coverage but don't have enough primary care doctors. Insurance does not equal access.
To produce more family physicians, we need to resolve the "income differential" between primary care doctors and specialists, many of whom make 2-3 times more than FPs. There is simply no way to increase the number of family physicians when medical students see how much more they can make by going into a specialty instead.
CMS (Centers for Medicare and Medicaid Services) is looking into adjusting overvalued and undervalued CPT codes and has been criticized by specialists who see a loss of income. To counteract this, Heim said we need to write to our legislators to voice support for CMS's efforts.
For instance, some cardiologists claimed that eliminating the consult code would cause them to lose so much income that they would have to stop practicing cardiology and go back to primary care.
"That's okay, I said. They can come to my office and I'll teach them how to be a primary care doctor. Let's see how they like that," Heim said.
She pointed out that we need to bring Medicaid reimbursements up to at least the level of Medicare. "When you're losing money on visits, increasing the volume doesn't help."
Administrative simplification also needs to happen to relieve the crushing red tape and bureaucracy that every primary care doctor has to deal with.
Dr. Heim listed some of the major highlights of the current proposed legislation:
CMS (Centers for Medicare and Medicaid Services) is looking into adjusting overvalued and undervalued CPT codes and has been criticized by specialists who see a loss of income. To counteract this, Heim said we need to write to our legislators to voice support for CMS's efforts.
For instance, some cardiologists claimed that eliminating the consult code would cause them to lose so much income that they would have to stop practicing cardiology and go back to primary care.
"That's okay, I said. They can come to my office and I'll teach them how to be a primary care doctor. Let's see how they like that," Heim said.
She pointed out that we need to bring Medicaid reimbursements up to at least the level of Medicare. "When you're losing money on visits, increasing the volume doesn't help."
Administrative simplification also needs to happen to relieve the crushing red tape and bureaucracy that every primary care doctor has to deal with.
Dr. Heim listed some of the major highlights of the current proposed legislation:
- No public option. Instead there will be state by state insurance exchanges.
- 10% bonus for primary care.
- 94% of population will be covered under the Senate plan.
- Establishment of a Medicare Advisory Board.
- Accountable Care Organizations.
- Dependent coverage up to age 26.
Heim acknowledged that the current bill is not perfect but that "it has a lot more good than bad," adding that healthcare reform will be an ongoing process.
-----------
I will be meeting with my state assemblymember and state senator on Monday to lobby/discuss CAFP's position on various pieces of healthcare legislation making its way through the state Capitol. We all complain about how bad the system is. This is my chance to try to do something about it.
If you want to do something about healthcare reform, you can help by:
As Dr. Tom Bent, CAFP's president said, "We no longer have the luxury of hiding in our exam rooms, or of just being a good doctor. We have to learn how to talk to the Rotary Club, legislators, the news media and the public."
Blogging's good, too, I assume.
I will be meeting with my state assemblymember and state senator on Monday to lobby/discuss CAFP's position on various pieces of healthcare legislation making its way through the state Capitol. We all complain about how bad the system is. This is my chance to try to do something about it.
If you want to do something about healthcare reform, you can help by:
- Voting
- Writing to your legislators
- Writing a letter to the editor of your local paper
- Asking your patients to write to their legislators or local papers
- Posting/linking/tweeting/blogging about healthcare reform
- Contributing to FP-PAC, CAFP's Political Action Committee (or your own state's PAC) or FamMedPac, AAFP's PAC so that someone will speak to the legislators for you besides the lobbyists for the insurance and drug companies.
As Dr. Tom Bent, CAFP's president said, "We no longer have the luxury of hiding in our exam rooms, or of just being a good doctor. We have to learn how to talk to the Rotary Club, legislators, the news media and the public."
Blogging's good, too, I assume.
Wednesday, February 24, 2010
A Sign of the Times
Aaron Blackledge, MD, of CarePractice in San Francisco has a message that he would like to share with the public about the current state of the healthcare system.
Being a primary care doctor these days is becoming more and more discouraging with the current payment system and insurance hassles, so much so that doctors are working less hours as noted in this Washington Post article:
Average hours dropped from about 55 to 51 hours per week from 1996 to 2008, according to the analysis, appearing in Wednesday's Journal of the American Medical Association.
That's the equivalent of losing 36,000 doctors in a decade, according to the researchers. And it raises policy questions amid a looming primary care doctor shortage and Congress considering an expansion of health insurance coverage that would mean more patients.
It's not hard to figure out why.
The overall decrease in hours coincided with a 25 percent decline in pay for doctors' services, adjusted for inflation. And when the researchers looked closely at U.S. cities with the lowest and highest doctor fees, they found doctors working shorter hours in the low-fee cities and longer hours in the high-fee cities.Unless there is meaningful healthcare reform soon, things will probably get worse before they get better.
Saturday, February 20, 2010
New Look
The weather is starting to warm up a little. Spring is in the air. It was about time I spruced up the place.
But mainly it was because the old commenting system I used (Haloscan) went kaput, and I wanted to implement Blogger's commenting system in its place. All the old comments got trashed (sorry) but I had no control over that. Give the new layout a spin. Make some new comments. Click on some links. Go wild while we're waiting for healthcare reform to happen. Yep, any time now.
But mainly it was because the old commenting system I used (Haloscan) went kaput, and I wanted to implement Blogger's commenting system in its place. All the old comments got trashed (sorry) but I had no control over that. Give the new layout a spin. Make some new comments. Click on some links. Go wild while we're waiting for healthcare reform to happen. Yep, any time now.
NCQA wants your opinion
The National Committee for Quality Assurance, better known as NCQA, wants to know what you think are the most important features are of the Medical Home. Go to this link and tell them.
Personally, I thought these listed features were all important, but narrowed it down to my top 5:
Personally, I thought these listed features were all important, but narrowed it down to my top 5:
- wait time
- seeing the same doctor or nurse
- listens and answers your questions (well, duh!)
- knows you well
- access to help without making a visit
Some of these seem so basic, it makes me wonder why they even have to ask.
Wednesday, February 17, 2010
Happy Anniversary
Ben Chan, a family physician, has just opened his new solo practice and writes:
It has been 8 years since I read Gordon's article. Now, I am sitting in my office in this opening day, waiting for the first patient to call and make an appointment. So this is what you all went through. Emotionally, it has been like a roller coaster ride. At one time, I am happy that I made this tiny leap. On the other hand, there are times when I kick myself and ask, "What are you doing?" For now, only time will tell. At least, at the end of my career, I can tell myself that I tried!
Coincidentally, it was 6 years ago today that I first opened my little office for business. I remember the open house I had on Valentine's Day 2004 to celebrate my new solo venture. We handed out chocolates and flowers and ordered way too much food. On my first day of business, I sat by the phone and waited and waited . . . and waited. I felt like I couldn't leave the office because what if somebody called? I was afraid of missing them. But no one called.
The days passed, with no patient in sight. I knew it would be slow to start but yeesh— not this slow. I brought no patients with me from Kaiser and was new in the medical community. I placed some ads in the local paper. I asked friends to tell their friends. It was lonely.
Finally, 2 weeks later, on March 1st, I saw my first patient. I saw him at 8PM, and he had no insurance and forgot to bring cash. I remember that he felt embarrassed and offered to go to the ATM up the street so he could pay me. I felt bad because it was raining, but I thought to myself, I did just provide medical care for him and if he didn't pay me now, who knew when I would ever see him again? Would he even come back after he left?
He did come back and paid the $40 for my first visit. Six years and 5000+ visits later, I just did the 2 month old well child check for his 2nd son. He still doesn't have insurance, but I'll always remember who my first patient was. So will Ben.
And Ben shouldn't belittle his accomplishment by referring to it as a "tiny leap". It is a huge leap of faith to leave the safety of a traditional group practice and go it alone. Some would say, it's crazy. But it's like that old Apple commercial:
Here'’s to the crazy ones. The misfits. The rebels. The troublemakers. The round pegs in the square holes. The ones who see things differently. They’re not fond of rules and they have no respect for the status quo. You can praise them, quote them, disagree with them, glorify or vilify them. About the only thing that you can’t do is ignore them. Because they change things. They push the human race forward. While some may see them as the crazy ones, we see genius. Because the people who are crazy enough to think that they can change the world, are the ones who do.
So here's to many more physicians like Ben who are trying to change THE world by changing THEIR world. It has certainly changed mine for the better and, I hope, the lives of the patients whom I have seen in my little micropractice.
Go get 'em, Ben.
Wednesday, January 20, 2010
This would be funny except that it's true

From Candorville.com
Unfortunately, the Republican win in the Massachusetts Senate election probably means that these kinds of shenanigans will keep happening.
Tuesday, January 19, 2010
Rochester, NY: IMP Capital
Anyone who has been following my blog won't find this article from today's Rochester Democrat and Chronicle unusual:
What is unusual is that this article points out that there are 8 Ideal Medical Practices in this local area, which is frankly amazing considering how few IMPs there are in the entire US.
Other IMP clusters are located in Seattle, Portland (OR), Southern California, Albuquerque, Albany, St. Louis and New York City.
For a list of IMPs around the country, go to www.impmap.com. Don't forget to use the zoom in/out controls to take a closer look.
When Dr. Linda Lee sees patients, she brings them from the waiting room, typically spends a half hour with them, cleans up the exam room and submits the insurance claims online. She's the one who returns phone voicemails, and she gives patients her cell phone number for urgent after-hours needs.
She has no nurse, no billing staff and no answering service. She only has a part-time secretary to digitally scan records that still arrive on paper at her paperless office.
The Rochester family physician's 5-year-old, low-overhead, solo practice is a stark contrast to the hurry-up, assembly-line format she found in large medical practices. "You basically had to see a patient every 10 minutes," said Lee. "How can you address the patient's medical problems in that short a time?"
What is unusual is that this article points out that there are 8 Ideal Medical Practices in this local area, which is frankly amazing considering how few IMPs there are in the entire US.
Other IMP clusters are located in Seattle, Portland (OR), Southern California, Albuquerque, Albany, St. Louis and New York City.
For a list of IMPs around the country, go to www.impmap.com. Don't forget to use the zoom in/out controls to take a closer look.
Sunday, January 10, 2010
Those Who Can't Blog, Link
So even though I haven't been keeping up with my blog, I thought I should point out some excellent bloggers who not only manage to write something on a regular basis, but also have something meaningful to say.
The Ideal Medical Practices Blog's focus is on the myriad problems facing America's healthcare system and especially its beleaguered primary care physicians, and what can be done to bring about real change.
Dr. Malia Reckons are the insights and thoughts of a solo family doctor in Rochester, NY, whose practice model is very similar to mine.
I just discovered that The Examining Room of Dr. Charles has re-opened after a two year absence. "Dr. Charles" is a unique voice in the blogosphere, whose tales about medicine and life in general are more like finely crafted works of art. I highly recommend his site.
Finally, while not a blogger, Dr. Atul Gawande is clearly an excellent and insightful writer who also happens to be a general and endocrine surgeon. His recent article for The New Yorker echoes my thoughts on how no single solution to our healthcare crisis is possible, namely because nobody knows which approach will work. He argues that, like in America's early agricultural industry, pilot programs may help guide us out of our national dilemma. After all, when you don't know which way to go, why not try several different directions at the same time instead of just one?
The Ideal Medical Practices Blog's focus is on the myriad problems facing America's healthcare system and especially its beleaguered primary care physicians, and what can be done to bring about real change.
Dr. Malia Reckons are the insights and thoughts of a solo family doctor in Rochester, NY, whose practice model is very similar to mine.
I just discovered that The Examining Room of Dr. Charles has re-opened after a two year absence. "Dr. Charles" is a unique voice in the blogosphere, whose tales about medicine and life in general are more like finely crafted works of art. I highly recommend his site.
Finally, while not a blogger, Dr. Atul Gawande is clearly an excellent and insightful writer who also happens to be a general and endocrine surgeon. His recent article for The New Yorker echoes my thoughts on how no single solution to our healthcare crisis is possible, namely because nobody knows which approach will work. He argues that, like in America's early agricultural industry, pilot programs may help guide us out of our national dilemma. After all, when you don't know which way to go, why not try several different directions at the same time instead of just one?
Monday, January 04, 2010
Subscribe to:
Comments (Atom)